The 35th research award from the Okinawa Medical Research Foundation
Assistant professor Miki Higaonna, PhD, RN, PHN has received the 35th research award from the Okinawa Medical Research Foundation [Okinawa Ikagaku Kenkyu Zaidan] in February, 2021. Her contribution to research studies focusing on nursing practice and patient health outcomes relating to patient safety and to publish original research articles in internationally recognized journals were highly regarded from the foundation. Following are the selected publications by Dr. Higaonna.
1. Predictive validity of a modified Japanese Nursing Association fall risk assessment tool
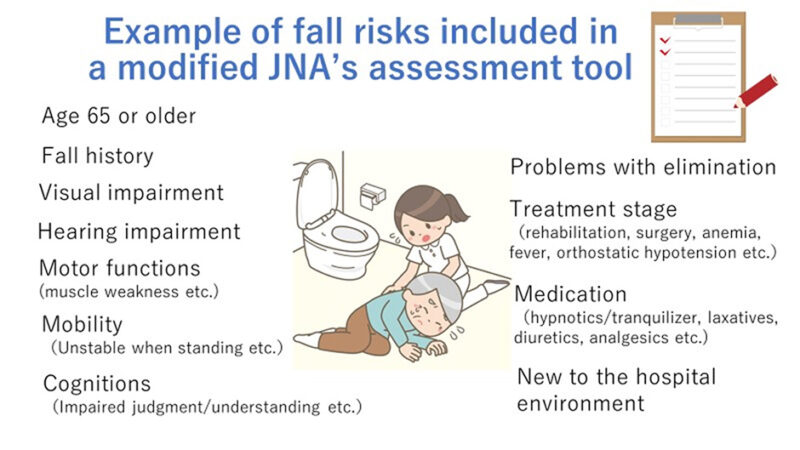
Nursing has an important role on prevention of inpatient falls, and inpatient falls are considered as an indicator for a quality of nursing practice. Most Japanese acute hospitals employees fall risk assessment tools, which include several fall-risk factors, to assess their patients’ fall risks, and nurses conduct the assessment for all inpatients. In this retrospective cohort study, the predictive validity of a modified Japanese Nursing Association’s (JNA’s) fall risk assessment tool was evaluated and compared at different observation periods: 7-, 14-, 21-, and 28-days in a 600-bed university hospital. The study has shown that the predictive validity of the tool was good enough to be used in the study hospital. The study has also shown that predictive validity in the 7-day observation sample was significantly higher than the 14- and 28-day samples, but no significant difference was found relative to the 21-day observation sample.
Reference:
Higaonna M. (2015). The predictive validity of a modified Japanese Nursing Association fall risk assessment tool: A retrospective cohort study. International Journal of Nursing Studies, 52(9), 1484-1494.
Access to this journal article: https://doi.org/10.1016/j.ijnurstu.2015.05.009
2. Development of an evidence-based fall risk assessment tool and evaluation of interrater reliability
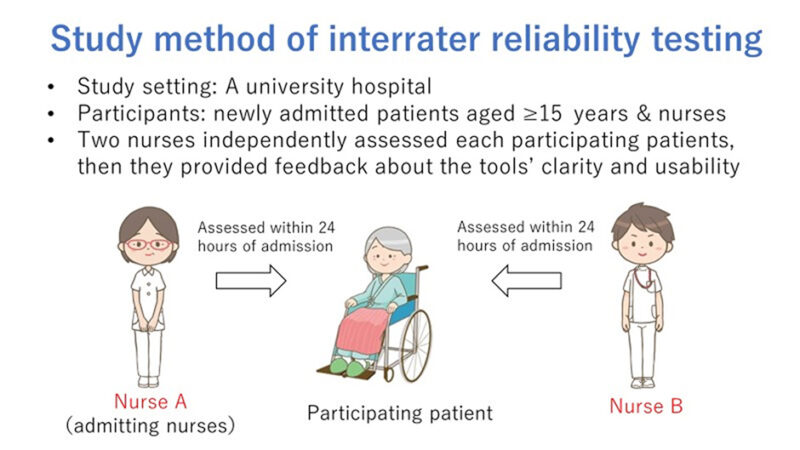
We developed a fall risk assessment tool (11 risk factors comprising of 23 items) based on a literature review and expert discussion. Then, we tested the tool’s interrater reliability by asking two nurses out of a possible 125 nurses to independently assess each participating patients (n = 114) on admission day. Twenty-one items showed perfect or substantial agreement. However, the study has indicated that the items of elimination and cognitive impairment require further modification because of their suboptimal interrater reliability or unclarity and difficulty reported by the participating nurses.
Reference:
Higaonna M., Enobi M., & Nakamura S. (2017). Development of an evidence-based fall risk assessment tool and evaluation of interrater reliability and nurses’ perceptions of the tool’s clarity and usability. Japan Journal of Nursing Science, 14(2), 146-160.
Access to this journal article: https://doi.org/10.1111/jjns.12144
3. Nursing delivery models and patients’health outcomes
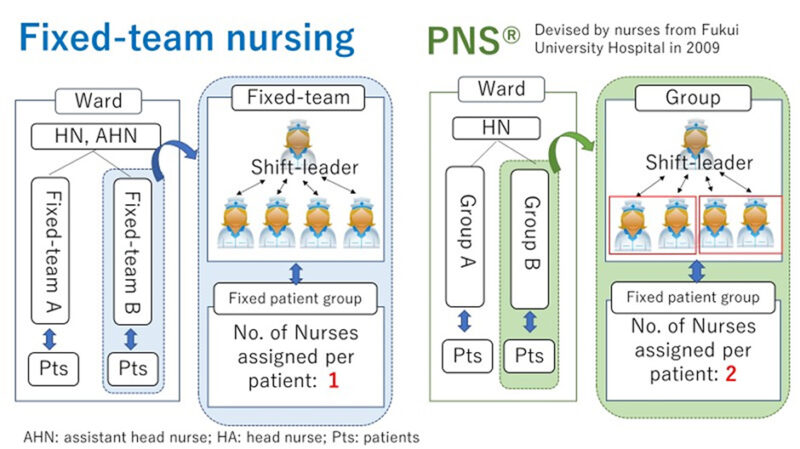
This retrospective cohort study examined the association between nursing delivery models and patients’ health outcomes (30-day in-hospital mortality and functional decline) using the data from the Diagnostic Procedure Combination database, routinely collected health data for Japanese administrative claims. The study included two nursing delivery models commonly used in Japanese acute hospitals: fixed-team nursing model and Partnership Nursing System® (PNS®). The number of nurses assigned per patient per shift was one in fixed-team nursing vs. two in PNS®. The study showed no statistically significant association between the nursing delivery models and 30-day in-hospital mortality. However, the PNS® group was found to have a higher proportion of patients with functional decline than the fixed-team nursing group (p = 0.03).
Reference:
Higaonna M., Morimoto T., & Ueda S. (2020). Association between nursing care delivery models and patients’ health outcomes in a university hospital: A retrospective cohort study based on the Diagnostic Procedure Combination database. Japan Journal of Nursing Science, 17(2), e12319.
Access to this journal article: https://doi.org/10.1111/jjns.12319